Drugs and devices
On the diabetes superhighway it is crucial to control blood sugar levels

According to the WHO, there are approximately 422 million people with diabetes in the world, and this number is expected to rise to 520 million by 2030. It is estimated that 1.6 million deaths are directly attributed to diabetes each year.
The incidence of diabetes in Portugal has been increasing in recent decades. Data from 2015 show that diabetes affects about 13.3% of the population aged between 20 and 79, that is, more than 1 million Portuguese. Portugal is therefore one of the European countries with the highest prevalence rate of the disease.
Yes, the numbers are staggering and continue to grow every year.
It is believed that about 75% of people with diabetes do not have adequate control of their disease, which leads to an increased risk of health complications in people with type 1 or type 2 diabetes.
It is therefore essential to control these patients’ glycaemia adequately, thus reducing the morbidity and mortality associated with diabetes, as well as the costs for society and economy.

What is glycaemia?
The concentration of glucose in the blood is called glycaemia. The unit of measurement used in Portugal is mg / dL
The reference values for blood glucose in healthy people are:
-
On an empty stomach: between 70-100 mg / dL
-
Postprandial (1h30 to 2h after a meal): up to 140 mg / dL
The above figures are reference values only. You should talk to your doctor about the glycaemic control goals he has set for you.

Diabetes and glycaemia monitoring
Diabetes is a disease characterized by persistent hyperglycaemia (high blood glucose levels), which over time gives rise to metabolic changes that can cause serious damage to several organs; therefore, it is evident that glycaemic control, and, in particular, glycaemic self-monitoring are essential. This monitoring will reduce/avoid the onset of late complications of the disease (blindness, amputation, kidney, heart, brain problems ...), which greatly decrease the patients’ quality of life.
If you suffer from diabetes, discuss with your doctor the possibility of doing your own blood glucose monitoring.

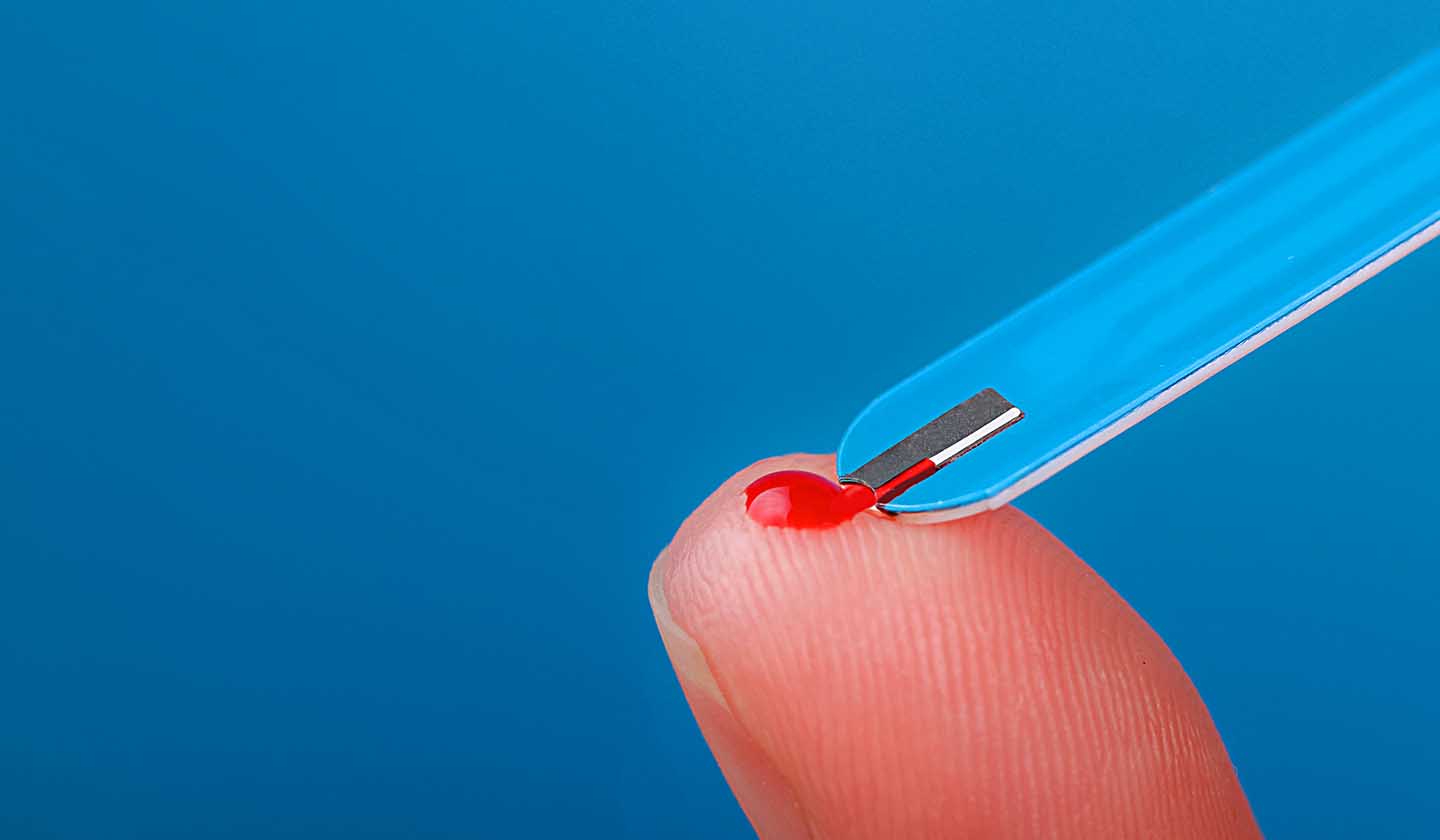
Self-monitoring of blood glucose (SMBG)
In this type of monitoring, the patient uses blood glucose meters (glucometers), which allow information on capillary blood glucose to be obtained in a matter of seconds.
There are several laboratories dedicated to the development of glucometers. These devices are increasingly accurate and simple to handle, so that they can be easily used by any patient. These devices are available free of charge in hospitals, health centres and pharmacies. However, you should always talk to your doctor first and discuss the benefits of getting a blood glucose meter. The device should be chosen according to the patient's characteristics (literacy, technological literacy, visual or hearing difficulties).
More recently, a system was developed for measuring blood glucose at any time, without the need for capillary puncture. It consists of a sensor that is placed on the forearm and a screen that allows the reading of the results.

SMBG (Self-Monitoring Blood Glucose) has several advantages:
- Provides real time information (this is important so that you can act both in situations of hyperglycaemia and hypoglycaemia);
- The capillary blood sample needed to perform blood glucose tests is small (in the case of glucometers);
- Glucometers are easy to use and, because they are small, they can be easily transported;
- Blood glucose meters can store a large amount of data related to blood glucose test results (with the associated day and time), thus giving information on average values and allowing to keep a record of blood glucose control which can be shared with the doctor.
- SMBG reduces the occurrence of hypoglycaemia (being especially important for patients who take insulin and use hypoglycaemic oral antidiabetics, because it allows to control glycaemia);
- Also, it allows us to adjust the therapy, exercises, and diet (for example, insulin) according to the results obtained;
Difficulties in using glucometers
Some difficulties may be experienced when using these devices, making it impossible for the patient to obtain results or leading to unreliable results. Most of the errors are the operator’s fault. Here are some examples:
- Incorrect storage of the test strips (they must be stored in dry, cool places and protected from direct sunlight);
- Use of test strips that are out of date (always confirm the expiration date on the packages);
- Performing the test with dirty hands (fingers);
- Dirty meter (traces of blood);
- Alcohol cleaning interference (let it dry well before pricking your finger; there is no need to disinfect, just wash with soap and water);
- Performing the test with an insufficient blood sample;
- Outside temperature too high or low when performing the test (blood glucose meters are accurate when used between 10 - 40 ºC);
Sources
iSaúde
Farmácia Distribuição Magazine
Também lhe poderá interessar
Sexuality
Erectile dysfunction was once a drama, today it is not
Endocrine system